As a Pilates teacher specializing in women’s health, I’ve spent years helping others rebuild strength after pregnancy and childbirth. But even with all my expertise, I’ve lived the challenges of Diastasis Recti (DR) firsthand. My recent surgery to repair my DR was a journey of empowerment, learning, and advocacy—with a few unexpected twists along the way. Here are five key lessons I’ve taken from the experience, and I hope they inspire other women to take control of their health and make informed choices.
1. The Postpartum System Is Broken, but We Can Demand Better
After childbirth, women in Ontario—and much of the world—are sent home with little more than a pat on the back and a newborn in their arms. There’s no physiotherapy, no guidance on how to move safely, and no support for healing. Meanwhile, in countries like Australia, funding for DR repair surgery and postpartum care is prioritized.
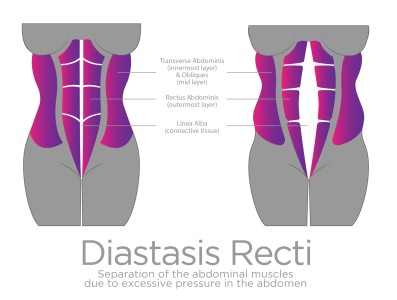
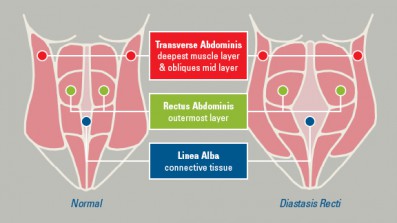
Why is childbirth treated as something we’re just supposed to endure? DR is dismissed as a cosmetic issue when the long-term effects of a weakened core can be debilitating. It’s time to demand better, not just for ourselves but for future generations of mothers.
2. Surgery Is Not “Cosmetic”
Let’s talk about the term “Mommy Makeover.” It trivializes what many women endure and reduces legitimate medical needs to something frivolous. A tummy tuck may reshape the body, but DR repair surgery restores function to a critical part of the body—your core. For me, this was about reclaiming my ability to live, work, and move without pain.
Elective or not, this surgery was a medical necessity for me. It’s time we shift the narrative and recognize that women seeking DR repair are advocating for their health, not chasing vanity.
3. Choosing Surgery Was Empowering—and a Little Magical
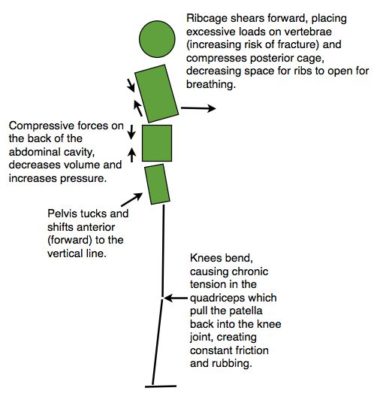
As someone deeply rooted in movement science, I knew my DR was significant. For years, I managed it with targeted exercises, building strength, and avoiding certain movements. But despite my best efforts, setbacks—like when I fell while picking up my son—became harder to recover from.
Around this time, something remarkable happened. I was starting to come to terms with the fact that surgery might be my best option. And then, out of nowhere, my surgeon appeared. Well, not out of nowhere—he was one of my Pilates clients! I couldn’t believe it. Here was this highly skilled surgeon specializing in abdominal reconstruction, sitting across from me as I explained core stabilization exercises. It felt like a sign—as though the universe (or my own determination) had manifested him.
Deciding to have surgery wasn’t easy, but meeting my surgeon made everything click. The empowerment I felt in taking control of my health was immense, and I hope every woman feels that same agency in making decisions for her body.
4. Living with DR Was a Constant Cycle of Progress and Pain
I lived with DR for years before deciding on surgery. I’ve felt the frustration of working hard, seeing gains, and then facing setbacks. From being bedridden after a setback to rebuilding my strength over six months, it was an exhausting cycle.
The reality is that managing DR requires an immense amount of dedication and effort. While I’m proud of the strength I built, I realized that I couldn’t keep training at this level forever. Surgery offered me a way to break the cycle and focus on moving forward.
5. Pain Is Pain, and Women Deserve Better
It’s easy to dismiss DR as a consequence of childbirth and tell women to “just live with it.” But pain is pain, and it deserves to be addressed. Why do we allow women to suffer in silence when solutions exist?
Women’s health is often swept under the rug, especially when it comes to postpartum issues. The differences between public and private healthcare, scheduled and emergency surgeries, highlight inequities that need addressing. Every woman should have access to the care she needs, regardless of her financial status.
6. The Cost Factor and Financial Tips
Let’s be honest: surgery can be expensive, and DR repair is often an out-of-pocket expense. In many places, this type of surgery isn’t covered by public healthcare because it’s considered elective (cue the eye roll). However, there’s a silver lining: in many cases, you can claim it as a medical expense on your taxes. It’s worth checking with your accountant or financial advisor to see if this applies to you.
While the cost might feel like a hurdle, remember that this is an investment in your health, well-being, and future. For me, it was about weighing the short-term expense against the long-term relief and empowerment I’d gain
Moving Forward: Empowerment Through Advocacy
My DR surgery wasn’t just a physical repair; it was a step toward reclaiming my health, my strength, and my life. It’s a decision I made for myself, and I’m proud of it. But I’m also determined to use my voice to advocate for better postpartum care for all women.
If you’re considering DR surgery or feeling stuck in the cycle of managing symptoms, know that you’re not alone. Educate yourself, trust your instincts, and seek support. Together, we can break the silence around postpartum health and demand the care and respect women deserve.
Oh, and if you’d like to hear more, I recently joined Nikki Bergen on her podcast We Go There to talk all about my journey, women’s health, and the advocacy we both believe in so deeply. You can find the episode on her website SOON for the launch of Season 11. It’s an incredible platform, and I’m so grateful to Nikki for creating a space where these conversations can happen.




 You’ll notice there are a lot of foods that overlap in various categories. Whole foods are loaded with a variety of vitamins and minerals that benefit the body in more ways than one. It doesn’t have to be complicated! The key is to include mostly real foods and to limit processed, packaged foods as much as possible – and don’t stress about the odd treat here and there either!
You’ll notice there are a lot of foods that overlap in various categories. Whole foods are loaded with a variety of vitamins and minerals that benefit the body in more ways than one. It doesn’t have to be complicated! The key is to include mostly real foods and to limit processed, packaged foods as much as possible – and don’t stress about the odd treat here and there either!