KELSEY’S STORY – A “Missed” Miscarriage
About a year after we were married, we had a candid discussion about when we’d “try” to have a baby. What is good timing for us, are we ready financially and willing to give up our current lifestyle for something different.
A few months after that conversation, I found out I was pregnant. It happened fast and it came with a plethora of emotions from so excited to so terrified.
Since the timing fell on Christmas, we started telling family around the 7-week mark. I even bought cute shirts for my niece and nephew that said: “we’re going to be big cousins”. I would later tell my sister to burn these.
Just after Christmas, we were sent for a dating ultrasound and like fresh new parents, we showed up thinking we could both go in the room and experience a “movie-like” first ultrasound moment. Anyone who has had a maternal ultrasound knows it’s anything but. After the first few parts of the scan, my husband was invited in and we were shown the little blob on the screen and the tech even turned up the volume to hear the heartbeat. I remember thinking it sounded slower than I imaged but didn’t think much more about it.
That next day we headed up North to visit family and spread the good news that way. I’ll never forget that while telling my in-laws, my doctor called me and interrupted that moment of joy for the first-time grandparents-to-be. I could tell in my doc’s voice something wasn’t right but she was trying to remain positive. The baby’s heart rate was low, 76 to be exact, and we’d have to give it another week to see if it sped up. The doctor said that many times 7 weeks is too early to hear a proper heartbeat, but she also warned that I might miscarry if something was actually wrong.
That week felt like one of the longest weeks of my life.
I returned to the ultrasound clinic the following week, husband in tow, feeling so nervous and unsure of what was next. I didn’t miscarry in that week of waiting and I had read every single article on the internet and tried to convince myself that everything was going to be fine.
It was not.
As I was getting the ultrasound (the internal one, at that) I saw the tech’s face drop and tears started rolling down her cheeks. They’re not supposed to show emotion but I guess this one couldn’t help it. The baby had no heartbeat and I was sent home.
It’s almost impossible to explain the sadness, regret, guilt, and confusion that came afterward. We got a call from my doctor, who said it wouldn’t have been a viable pregnancy and that it’s very common so not to worry, we’ll get pregnant again quickly. She said it’s my body’s natural way of knowing that a baby won’t be viable. Not exactly the words of kindness I was looking for, but she booked us in at Mount Sinai’s early pregnancy loss clinic and that was that.
We arrived at the clinic the very next day to discuss our options. This is where we met Fran, a nurse who is an angel from heaven, who made one of the worst situations of our life, just a little bit less shitty.
We found out I was having what is called a missed miscarriage which means the baby has died but my body has yet to catch on, hence why I didn’t start bleeding or cramping or anything and still felt completely pregnant, hormonal and hungry (SO HUNGRY). My options were to wait and naturally pass the embryo, take misoprostol, a drug that induces a miscarriage or have a D&C (dilation & curettage), a surgical procedure where they scrape out your uterus when you’re under general anesthetic.
It felt like I was choosing the best way to die. We went with the pills to bring on a miscarriage since they didn’t have surgical time available until a week later. I couldn’t face another day pregnant and just wanted to get it over with.
That night, I took misoprostol and had a miscarriage at home. I wouldn’t wish that experience on my worst enemy. I had contractions similar to labour for about two hours until I passed what I later learned was the embryo.
The experience changed me a lot. All of this was completely new and I didn’t know at the time but we went on to struggle to get pregnant again. I felt some of the lowest lows I’ve ever experienced in my life with moments where I didn’t believe I would ever feel happy or okay again.
I also ironically had a friend who was pregnant a few weeks away who I watched through an entire pregnancy I knew I wanted so bad and didn’t have. I avoided baby showers, social events and while trying to be happy for friends and acquaintances who were getting pregnant, what seemed like every second day, I was so sad for myself that it was really hard. In hindsight, I wish I had handled it better but at the time I was incapable.
I went to therapy to help wrap my head around everything that happened and I also began being really open about the experience. I’ve come to realize that I hate the 12-week announcement rules put on women. It makes no sense that those suffering a miscarriage before 12 weeks should have to suffer silently. I think that stigma should be broken and we should, if we’re comfortable, speak openly about this real thing that happens to SO many women.
If you know someone who has had a miscarriage or is going through it currently, my suggestion would be to just be there to listen but also give them the space they need. It takes a toll on your body and mind, so sending food or a nice gift of self-care is always a thoughtful way to show you’re thinking about them. Also, don’t be afraid to ask how they’re doing, it really does sometimes feel like people who haven’t been through it don’t quite get the weight of it and that can be tough, especially with close friends.
If you’re reading this and you’re struggling, be gentle with yourself. It’s so easy to spiral down a path of blaming yourself or searching for a reason for why something like this happened; I exercised too much, I’m not healthy enough, I found out late and had one too many glasses of wine.
It is not your fault.
The other thing we did is planted a tree in our backyard on what would have been our due date, it was a really nice way to honour the loss.
The last thing I will say is to lean on your community or find a community you can lean on. After my miscarriage when we went on to struggle with infertility, I found an app called Kindara with a community of women who were also struggling. Many of them also experienced loss and it really helped give me a place to be honest and open about how I was feeling and how much I was struggling.
The bottom line is you don’t have to suffer alone because you aren’t alone. The stats are one in four pregnancies end in miscarriage. My miscarriage was on January 4, 2017, and I sit here now with hindsight watching my healthy 1-year-old rainbow baby, knowing that my life has happened just as it should.
 Time eventually heals. I still think about what might have been, especially when I look out at my beautiful Japanese Maple in my backyard. This experience has given me a new perspective.
Time eventually heals. I still think about what might have been, especially when I look out at my beautiful Japanese Maple in my backyard. This experience has given me a new perspective.
Above all, be kind to people because you really never know what they’re going through.
FLORENCE’S STORY – An Ectopic Pregnancy
I experienced pregnancy loss, just a month before my 24th birthday. I had just adjusted back to the city life after living abroad in Costa Rica where I had completed my yoga teacher training. My boyfriend at the time, traveled lots and was often away for work. On the day that I took myself to the hospital, he was in the Arctic and was only available via a satellite phone.
At the age of 23, I was not attempting to conceive, but it happened and I was unaware it had until I was actively experiencing the loss of my pregnancy.
I was 5 weeks pregnant when I discovered I was in fact miscarrying and not just experiencing another unusual menstrual cycle.
After a week of bleeding and waking to persistent cramps, I finally took a pregnancy test, as I suspected I could have been having a miscarriage. The + sign shortly appeared and I took myself to the ER, alone.
I brought myself to the ER around 6am, had multiple interactions with nurses and doctors that were not pleasant by any means. The nurse who drew my blood asked me what type of birth control methods I had used in attempt to prevent this “mistake”, implying that I was young and irresponsible. I will never forget that exchange.
After imaging and horrendous abdominal pain, it was concluded that I had had an ectopic pregnancy and I needed surgery immediately as it was a dangerous situation. I remember the technician telling me to sit down after my internal ultrasound, and I knew exactly what was happening by the expression on her face.
At this point, I called my sister who came to hold my hand as I was taken up the OR, by the same nurse who had previously interrogated me. It wasn’t until I met my surgeon that I felt safe. When I came out of the elevator I was greeted by a compassionate face and the words “I’m so sorry for your loss”

It all felt so shameful, frightening and abrasive.
I choose to remember the warmth of my doctor’s voice and the kindness of the anesthesiologist as I went into the OR. Throughout the hours at the hospital they were the first to recognize and acknowledge my pain and loss. They made me realize that I had not even processed what I really had lost.
This experience changed the entire trajectory of my life and career. I can remember sitting with a friend, weeks afterwards trying to process what had happened. I felt confused about grieving the loss of something I only had moments to connect to. She told me “this is happening for you, not to you”. Experiencing this early pregnancy loss has prompted me to advocate for women’s health. I figured, if I felt lost after my loss, so many other people must be feeling the same or worse. The lack of continuity of care following my loss was disappointing and frustrating. This gap in the healthcare system is what motivated me to specialize in the after care and postnatal care. It was a tough way to learn, but my loss has provided me with a compassionate heart and special understanding of what women enduring miscarriage are feeling. So I guess you could say, I made this traumatic experience something that happened FOR me – rather than TO me.

My advice for people looking to support someone going through a miscarriage is to show up. Just show up and be there. Don’t talk, give unsolicited advice or words of wisdom. All you can do is show up, physically, listen and offer love. Ask them what they need, and follow through with it. They may not know what they need, so in that situation just offer them love and a safe space to cry and process
For women who are struggling with pregnancy loss: You are not alone. As soon as I experienced pregnancy loss and I started to talk about it, I realized this. In fact, 1 in 4 women experience a miscarriage. Take the time you need and know that there is support. PAIL is an amazing organization out of Sunnybrook hospital in Toronto, that offers free counselling for early pregnancy and infant loss. They have expanded beyond Toronto and offer counselling over the phone too! Women are incredibly powerful, when we gather together it can be the most therapeutic gift – don’t be afraid to ask for help.
LYDIA’S STORY – Late Pregnancy Loss
I was 20.5 weeks along when we went for my anatomy ultrasound. We were told we were having a baby boy! He was looking totally healthy and growing according to schedule. We were so excited. Of course I went straight to the mall and started shopping!
I had booked a vacation for the following week with a girlfriend of mine… my last vacation before becoming a mom. We decided on a Caribbean cruise. My husband at the time didn’t like to travel, so she and I went alone.
Everything started out perfectly. We ate, we hung out by the bar drinking virgin cocktails – it was a lot of fun. I remember the exact moment things started to turn. I was sitting at a bar and felt like I had to go to the washroom. I tried and I couldn’t. I went to see the doctor on board. He tested my urine and found a high red blood cell count. He listened to the baby’s heartbeat and gave me a prescription for a bladder infection. I was way too nervous to take meds from a random doctor so I avoided it until I could chat with my own in the morning.
The next morning we were in port in Puerto Rico. We decided to get off and go shopping. My gf and I separated for a bit at a mall and I was stocking up on the cutest baby clothes. I remember feeling like I had to sit down. I wanted to curl up because my stomach was bothering me. I again thought I had to go to the washroom but again no luck. We decided to go back to the ship. I decided to call my doctor.
My doctor told me the chances of it being anything serious this far along were maybe 3%. He told me I could ride it out and see him 3 days later after the cruise, or I could miss the rest of the cruise and go to a hospital. Obviously I thought the odds were in my favour, so I carried on with the cruise. After numerous attempts to use the washroom and just not feeling right I went to lie down in the room. My gf went to the gym.
One final attempt to use the washroom was the worst moment I can ever remember. Blood. So much blood. Clots of it. I started screaming. I remember crawling to the phone. Dialing the doctor. Screaming I was in so much pain. I was alone. They sent a wheelchair and rushed me down. The doctor asked for another urine sample and I couldn’t even stand up. I crawled to the toilet and my water broke. I just remember screaming and everyone rushing around. They checked my baby boy’s heartbeat which was still there. They gave me a shot for the baby’s lungs and called my husband. I knew what was happening. I was losing this baby.
The doctors decided I need to be in a hospital. There was no longer a heartbeat. My baby boy was gone. I made it to the hospital in Puerto Rico on Halloween night – one of the busiest nights of the year. I eventually saw a doctor and we decided the best thing to do was for me to give birth.
I was induced that night and delivered my beautiful baby boy the next day. I remember how small his perfect little body was. I said my goodbyes though many, many tears. His body was cremated and his tiny ashes are with me.
I have never felt so empty, sad or heartbroken in my life. I still remember every detail from that experience. I remember how I felt and how long it took me to move on.
Talking about it helped a lot. Surprisingly many people contacted me that they too had experienced similar loss. I was shocked actually. I didn’t feel so alone and it helped me move forward and keep trying.
I remember when we did try again to get pregnant, how every month that went by with a negative test, it sunk me. I was so disappointed, frustrated, hopeless. I didn’t think I was ever going to have a baby. In the big picture it was only about 8 months but that felt like an eternity. But I DID get pregnant again. Three beautifully, healthy girls as a matter of fact… within the next 4 years.
 I know my story is mine, and there are so many different ones out there. I have had other friends who have suffered pregnancy loss multiple times. My heart breaks for them. Any loss is still a loss no matter how far along someone is. Let them mourn. Let them feel what they need to feel and just be supportive. You may not know what someone is going through behind closed doors. Here’s to being kind to each other.
I know my story is mine, and there are so many different ones out there. I have had other friends who have suffered pregnancy loss multiple times. My heart breaks for them. Any loss is still a loss no matter how far along someone is. Let them mourn. Let them feel what they need to feel and just be supportive. You may not know what someone is going through behind closed doors. Here’s to being kind to each other.
LAUREN’S STORY – IVF Miscarriage
I went into my first round of IVF, full of hope, and convinced that it would work. After all, I already have a beautiful daughter, so my body knows what to do, right? Wrong! What I didn’t know was the depth of pain I was about to experience, and sadly, I’m not talking about the shots!
You see, I was under the impression that I was somehow in control. That if I took the medication, went to all my appointments, and switched up my diet, that everything would be fine. I read the books, took the vitamins, and purchased pineapple themed everything (pineapples are considered good luck for those going through fertility treatments).
I even repeated a mantra to myself every day, and I’m totally not a mantra person! Anyone who’s ever gone through IVF knows that it’s like playing the lottery, but you hear the success stories, and see the babies in people’s arms, and you never think that it’s not going to happen for you.
When the month finally arrived for our first frozen embryo transfer, I was so excited I could barely contain myself. I foolishly allowed my mind to wander and began to picture life with our new little bundle of joy. In September, we were officially considered PUPO (pregnant until proven otherwise) and began the dreaded two week wait.
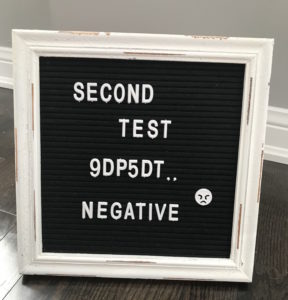
I went online to determine the best time to take a home pregnancy test, because I knew there was no way I would make it to the end of the two weeks. I discovered that the majority of women knew by six days post transfer that they were pregnant. So, on the evening of the 6th day, I took my first test. It was negative. I was discouraged, but I reminded myself that it was still early. I waited until nine days and then tested again, still no line. At this point, I’m not going to lie, I was pretty devastated. I figured this was it. It hadn’t worked.
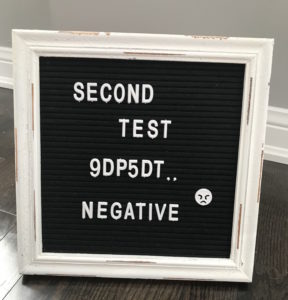
I had a follow up appointment for blood work the following day and was supposed to get a call in the afternoon with the official results. I remember that they called at lunchtime, and much to my surprise, the nurse said, “Congratulations! You’re pregnant!” I was in total shock. What? I was pregnant? How is this possible? My feelings instantly went from sad and depressed to over the moon. I texted my partner that he was finally going to be a Daddy, and he called me in tears. Little did we know what was in store for us.
 I returned to the doctor for standard blood work two days later and received a call that afternoon stating that my Beta hCG hormone was not doubling the way it should have. The nurse warned me that this could be a sign of an ectopic or chemical pregnancy, which would ultimately mean either surgery or a miscarriage. I felt as though I’d been punched in the gut. All the excitement drained from my body. She stated that it was still too early to tell, and that I was to return for blood work again, so that they could monitor my levels. So back I went in the morning, terrified that we would lose the baby we had been so desperately hoping for. That afternoon the nurse called to tell me that my hormone had increased but had not doubled, and that I was to return for a third test in a couple of days. I was anxious and scared, and yet still hopeful that things would turn around. Much to my surprise, they did. After my third blood test, the nurse shared that my hCG has started to double. I immediately felt relief. Like I could finally step off the emotional roller coaster I was on, and go back to being happy and excited for the future. I was scheduled for an ultrasound at six weeks where they would check on baby’s progress. Life returned to normal once again.
I returned to the doctor for standard blood work two days later and received a call that afternoon stating that my Beta hCG hormone was not doubling the way it should have. The nurse warned me that this could be a sign of an ectopic or chemical pregnancy, which would ultimately mean either surgery or a miscarriage. I felt as though I’d been punched in the gut. All the excitement drained from my body. She stated that it was still too early to tell, and that I was to return for blood work again, so that they could monitor my levels. So back I went in the morning, terrified that we would lose the baby we had been so desperately hoping for. That afternoon the nurse called to tell me that my hormone had increased but had not doubled, and that I was to return for a third test in a couple of days. I was anxious and scared, and yet still hopeful that things would turn around. Much to my surprise, they did. After my third blood test, the nurse shared that my hCG has started to double. I immediately felt relief. Like I could finally step off the emotional roller coaster I was on, and go back to being happy and excited for the future. I was scheduled for an ultrasound at six weeks where they would check on baby’s progress. Life returned to normal once again.
My partner and I went to the clinic on the day of the ultrasound together. We couldn’t wait to see our developing baby. I was ushered into the room and he was told that he would be able to join us shortly. As I laid down on the table, I remember a swirl of emotions hitting me and happy memories of the first time I saw my daughter on ultrasound came flooding back. But within seconds, I knew something was wrong. The ultrasound tech began hammering me with questions about my blood results and then repeatedly pushed down sharply on my stomach while demanding to know whether I was seeing my doctor later that afternoon. I asked her if my partner was going to be joining us, and she abruptly said, “No!” She told me to get dressed and to go see the doctor. I held back tears as I walked to the waiting. I whispered to my partner, “Something’s wrong,” before beginning to cry. We met with our doctor twenty minutes later and he shared that it looked like the embryo had moved to the opening of my left tube, and that I was likely experiencing an ectopic pregnancy. He gave us strict instructions to monitor for pain, and to go to a hospital if things became unbearable. My head was spinning as we left the office. How could this happen? Was it something I did? Or something I didn’t do? Would I end up needing surgery? Fortunately, I did not have to visit the hospital, but within a week I began to miscarry.
The next few weeks were some of my lowest. I felt alone in my suffering, even though I had people who loved and cared for me. I cried a lot, ate my feelings, and avoided leaving my house for anything other than work. I even missed my 20th high school reunion, because I just couldn’t bear to be around people. But slowly things got better and I felt the heaviness begin to lift. I went back to reading other people’s IVF journeys, and the triumphs they experienced after years of setbacks. I gained inspiration from their resilience and their drive to keep going. I refocused my energy on what I already had in my life, including a loving partner and an amazing daughter, and I reminded myself that I was strong, that I have been through a lot, and that I would get through this too!
My advice to others who are going through this:
- You are not alone, no matter how badly you feel. There are people who love you and want to be there for you. Let them!
- You will get through this! It may take a while, but eventually you will come out on the other side, and you will be amazed by your own strength.
- It’s okay to fall apart! Tears are cathartic. Venting is cathartic. Taking time for yourself is cathartic. Put yourself first and do what you need to do for you!
- This what not your fault. Nothing you did or didn’t do caused your miscarriage.
- If you know someone who is experiencing a miscarriage, check in on them. Send them a text or call to let them know that you’re thinking of them. Ask them if there’s anything you can do to help? They’ll likely say, “No,” but I can assure you that they will take comfort in knowing that you’re there.
KIM’S STORY – Recurrent Miscarriages
I didn’t particularly want kids but I also did not, not want kids. I was busy pursuing my acting and dancing career. I always figured I would just know if I wanted to be a mom and then I just would be one. Ha! Well what the hell did I know??
I found the “one” and that brought a lot of healing to the wounds in my heart. I began to feel like a big part of the human experience was to be a parent. I was sure I did not want to leave the planet without becoming one.
I started trying to have a baby at 35. By the time I was 39, I had gone through 8 miscarriages.
I got pregnant on our honeymoon when I was 36. By that point we had already had 4 losses. Conceiving on our honeymoon was like a dream come true. I was already considered ‘geriatric’ in the fertility world (that was fun reading on my chart). I knew I was only getting older and less fertile. Everyone kept telling me the quality of my eggs was diminishing.
After our honeymoon we went back to our clinic. It was official – we were pregnant. I had been taking progesterone suppositories to help the baby “stick”. The drugs were terrible. I would get so bloated, gaining up to 7lbs every month on them.
My HCG levels were doubling, so we went for our first ultrasound. There was baby, heartbeat and all. We literally could not believe it! The technician did mention the heartbeat was a little slow but not too bad – she would like it to go up at the next ultrasound.
I had several other ultrasounds, but one of them showed the heart rate starting to get slower. The baby had grown but the heartbeat not good. I was told the baby would not make it and I just needed to wait for it to pass. So every week I slowly watched the numbers get slower: 93, 84, 67 until finally my baby’s heart stopped beating. I was given misoprostol to start my uterus contracting so I could “birth” the baby. The cramps were indescribable. I remember lying on the couch and feeling what felt like a tennis ball literally fall out of my vagina. I knew what had happened.
I got up to the bathroom and there my baby was. You could see everything. Hands, head, feet, little body – even a placenta. That image will never leave my memory.
I asked my husband to bring the jar. After 4 previous losses, I had opted to bring this fetus in to be tested. Even after all my tests at the clinic, cycle monitoring, endless early morning blood work (I was a bartender so this was brutal), endless vaginal ultrasounds, hysterosalpingogram, small surgery to remove polyps in my uterus, a million progesterone suppositories and baby aspirin – nothing was actually deemed wrong with me, but yet everything was wrong with me. So in an act of desperation, I took my baby and carried it in my purse to the hospital for testing.
That day was beyond traumatic. I got lost, couldn’t find the lab and felt myself wanting to break down and cry while I trying to explain that I had my baby in my purse for testing and couldn’t find where I was supposed to go. Still, they could find nothing wrong with the baby.
It was really after this loss that I really got depressed. I gained weight and started giving up. I felt such shame, like a failure, like my body had failed me. I started really slacking on my health. I had done everything – seen the naturopath, done all the cleanses, changed my diet, acupuncture etc. I started being quite reckless. Needless to say this was not great for my marriage. After 4 years of sex on command and what felt like endless losses, we were in a dark place. I almost got to the place of accepting that I would probably never be a biological mother. We talked about adoption. We were open to exploring it.
I got pregnant again and lost. But 2 years later at 39, I got pregnant again and gave birth to my beautiful, healthy miracle baby daughter. Our hearts burst with joy!
 After our daughter was born, we weren’t sure if we should try to expand our family. There were so many factors: my age, finances, I was a sleep deprived wreck and still had a lot of injuries from my c section.
After our daughter was born, we weren’t sure if we should try to expand our family. There were so many factors: my age, finances, I was a sleep deprived wreck and still had a lot of injuries from my c section.
Then the unimaginable happened – I got pregnant again this year at 44. We were floored. For some naive reason, I let myself believe this was meant to be. My HCG numbers were doubling, pregnancy symptoms strong, I got to see our little bean on ultrasound… then nothing. No more growth, no more heart beat. I just had to wait for my baby to come out again. This one hit me so hard. I was mad at myself for believing it. I had been so worried about all the others, but for some reason I believed this time would work. We had started rearranging the house and making plans for a sibling. This was now my 10th pregnancy.
There were so many high’s and low’s on this journey. I largely felt alone, like I was living a double life – a life where I was secretly trying to have a baby, then secretly pregnant, then secretly miscarrying. I finally feel like I am in a place to share, connect, listen and help others. I really did feel shame. No one should feel that.
My advice to other women is hard to say because every journey is so unique. I wish I could tell you it’s going to work out, but the truth is I really don’t know. I want nothing more than for everyone on this journey to be blessed with a baby. Just know it’s not your fault. There is no shame in it. Your body is not a failure. You are not a failure. You are not alone. It is so much more common than you know. You are magical and a woman no matter where your journey takes you and you have a tribe of women rooting for you all the way. I’m screaming the loudest. xo

 You’ll notice there are a lot of foods that overlap in various categories. Whole foods are loaded with a variety of vitamins and minerals that benefit the body in more ways than one. It doesn’t have to be complicated! The key is to include mostly real foods and to limit processed, packaged foods as much as possible – and don’t stress about the odd treat here and there either!
You’ll notice there are a lot of foods that overlap in various categories. Whole foods are loaded with a variety of vitamins and minerals that benefit the body in more ways than one. It doesn’t have to be complicated! The key is to include mostly real foods and to limit processed, packaged foods as much as possible – and don’t stress about the odd treat here and there either!
 Time eventually heals. I still think about what might have been, especially when I look out at my beautiful Japanese Maple in my backyard. This experience has given me a new perspective.
Time eventually heals. I still think about what might have been, especially when I look out at my beautiful Japanese Maple in my backyard. This experience has given me a new perspective.

 I know my story is mine, and there are so many different ones out there. I have had other friends who have suffered pregnancy loss multiple times. My heart breaks for them. Any loss is still a loss no matter how far along someone is. Let them mourn. Let them feel what they need to feel and just be supportive. You may not know what someone is going through behind closed doors. Here’s to being kind to each other.
I know my story is mine, and there are so many different ones out there. I have had other friends who have suffered pregnancy loss multiple times. My heart breaks for them. Any loss is still a loss no matter how far along someone is. Let them mourn. Let them feel what they need to feel and just be supportive. You may not know what someone is going through behind closed doors. Here’s to being kind to each other.
 I returned to the doctor for standard blood work two days later and received a call that afternoon stating that my
I returned to the doctor for standard blood work two days later and received a call that afternoon stating that my  After our daughter was born, we weren’t sure if we should try to expand our family. There were so many factors: my age, finances, I was a sleep deprived wreck and still had a lot of injuries from my c section.
After our daughter was born, we weren’t sure if we should try to expand our family. There were so many factors: my age, finances, I was a sleep deprived wreck and still had a lot of injuries from my c section.




 It is only now that I understand how important certain aspects of her plan were – probiotics!! My children are now five years old and it’s only in the last two years that I’ve given more thought to how they were brought into the world, and how I was duped by the very care system in which I work. In retrospect, I was not given accurate information on what was in my babies’ best interest. Rather, I was offered a recommendation based on a biased perspective, one that medicalizes birth, disrupting our precious evolutionary fabric in the process.
It is only now that I understand how important certain aspects of her plan were – probiotics!! My children are now five years old and it’s only in the last two years that I’ve given more thought to how they were brought into the world, and how I was duped by the very care system in which I work. In retrospect, I was not given accurate information on what was in my babies’ best interest. Rather, I was offered a recommendation based on a biased perspective, one that medicalizes birth, disrupting our precious evolutionary fabric in the process. If you are pregnant, you may have googled – “safe exercises during pregnancy” – and what you likely found is overwhelming AND conflicting. So what are you to do? It’s important to seek out experts in the area of prenatal fitness, BUT also ask questions about their training, credentials and up to date research and education. We are frequently learning new information regarding exercise during pregnancy, so what may have been deemed a good idea a decade or even a few years ago has changed today.
If you are pregnant, you may have googled – “safe exercises during pregnancy” – and what you likely found is overwhelming AND conflicting. So what are you to do? It’s important to seek out experts in the area of prenatal fitness, BUT also ask questions about their training, credentials and up to date research and education. We are frequently learning new information regarding exercise during pregnancy, so what may have been deemed a good idea a decade or even a few years ago has changed today.