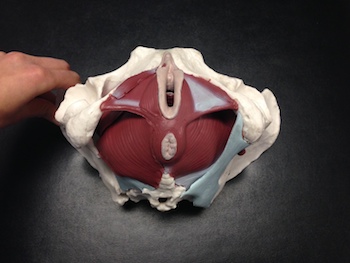
Hemorrhoids. I know, not the most glamorous topic. It’s embarrassing, some might even be horrified, but what I want to focus on is how normal and common these conditions of the pelvic floor are, especially after birthing a baby. Our bodies have gone through a lot, we did make a human!
Hemorrhoids are swollen veins in the lower part of your rectum or anus. The blood vessel walls of the vessels stretch, bulge, and get irritated. It causes rectal bleeding, especially with bowel movements.
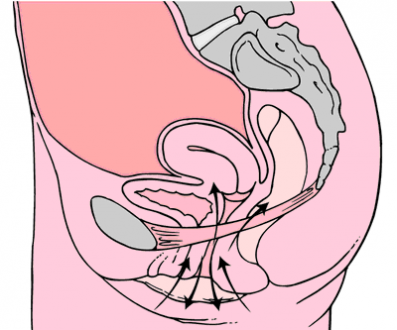
Technically, hemorrhoids are varicose veins of the anus. There are 2 main kinds of hemorrhoids; internal and external. Internal hemorrhoids are deep inside the rectum, they can’t be seen or felt. They are not usually painful but can bleed, and create a heavy sensation in the rectum. External hemorrhoids develop on the outside of the anus, so they can be seen and felt. They are more likely to cause symptoms of itching, pain, swelling, as well as bleeding.
Not fun… so, let’s just get down to the ways we can support our bodies and heal. As a reminder, please always consult with a healthcare provider.
Focus on fiber: That pelvic floor wants smooth and easy elimination. Think fruit, vegetables, whole grains, beans and legumes. A great breakfast choice can be a warm bowl of oatmeal with 1 tbsp of ground
flax seeds. Rich in soluble fiber which produces a gel-like substance when mixed with water that coats and soothes the digestive lining. This is very healing to the digestive system. I’d also suggest being mindful of dairy. Dairy is an inflammatory food and can contribute to constipation, which aggravates hemorrhoids. Aim for fiber-rich plant-based food options.
Up your fluids: My go-to’s are water and herbal teas. Sharing 2 herbs that offer medicinal benefits for varicosities and hemorrhoids, and are safe in pregnancy and breastfeeding.
Dandelion root is rich in minerals and acts as a diuretic, laxative, and digestive stimulant. It helps the digestive system by reducing gas, bloating, and constipation.
Chamomile tea, you can never go wrong with this herb. It clams the nervous system (hello multitasking mamas!) and contains tannins, a natural astringent, that helps tighten up blood vessels with anti-inflammatory benefits. A cup of tea a few hours before bed does the body good.
Think Bioflavonoids: These are a group of powerful phytochemicals created by plants that strengthen the walls of our veins. While there are dozens of bioflavonoids, the ones shown to help hemorrhoids are: rutin, hesperidin, and diosmin. These compounds improve the structure of veins, make them less susceptible to varicosities, and help hemorrhoids heal faster. Bioflavonoids have strong anti-inflammatory properties and they restore blood flow to tissues, reducing the bleeding in hemorrhoids. To say it quite simply they do a really good job of helping the situation!
Flavonoids are found in plants. Think color; citrus fruit, red peppers, berries, leafy greens, mangoes, broccoli, and red onions. Focusing on bioflavonoids is one of the best things we can do for hemorrhoids. Widely available in a supplement form, bioflavonoids are safe to take when pregnant or breastfeeding. This nutrient can be taken daily in a capsule with food and can be paired with vitamin C for maximum benefits. Brands to consider: Natural Factors Citrus Bioflavonoids, New Roots Citrus bioflavonoids, AOR C + bioflavonoids, Flora HemorAid
Probiotics: It’s believed that health begins in the gut, and the rectal area is the bottom end of the digestive system. So, to treat hemorrhoids, we need to work on gut health. Probiotics are very helpful to those with constipation, and when healing from hemorrhoids it is essential to ensure the smooth movement of the bowels. Eat a variety of fermented foods, kefir, kimchi, sauerkraut, and miso, and consider a supplement. Brands to consider: Genuine Health Women’s Probiotic, NFH Probio Sap or HMF Intensive.
Topical solutions: We often want to apply something to the area for immediate support.
Witch hazel: Can reduce both itching and pain, the two main symptoms of external hemorrhoids. It’s a natural anti-inflammatory, so it can also reduce swelling. It can be bought in a liquid form that you can apply directly to the hemorrhoids with a cotton pad.
Aloe: Very soothing to a painful area. It cools the inflamed tissue and helps it to heal. You can use the gel from the inside of a fresh plant, or buy a bottle of aloe gel from your local health food store.
Epsom salt baths: The salts are rich in magnesium which reduces inflammation and pain. Sitz baths have been shown to help alleviate the discomfort. Everything feels better after a good soak.
Lastly, and Nikki is your expert… we gotta move. We sit way too much. The Belle Method has you covered on this one.
Thank you for sharing your knowledge Dr. Rachel! You can learn more about her Naturopathic practice and doula services here on her website.